Acne is a chronic inflammatory skin disease that affects the majority of the population at some point in their lifetime. It usually starts at puberty and most of us in adolescence will have a few spots at some time. Acne is based in the sebaceous (oil-producing) glands that lie close to the hair follicles. These are most frequent on the face, neck, chest and back. Acne is therefore seen where these are common.
Acne can range in severity from non inflammatory lesions, seborrhea and comedones to more severe inflammatory acne and scarring.
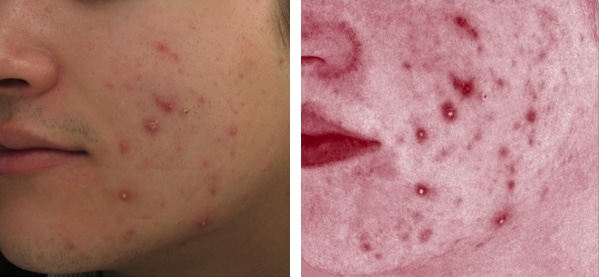
Inflammatory acne lesions can cause both physical and emotional pain and potential scarring. These photographs show how red and inflamed spots can become.
What causes acne?
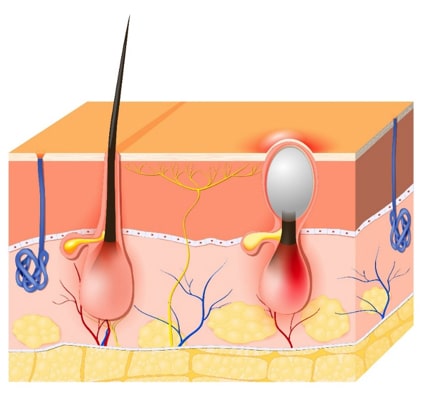
Acne is a disorder of the sebaceous glands. These glands are regulated by hormones and, more specifically, the androgens. Due to changes in hormones such as during puberty, the sebaceous glands produce more oil. More oil production leads to a series of events that can result in open and closed comedones – blackheads and whiteheads – and possibly papules and pustules – red, raised bumps and pus-filled pimples.
The sebaceous glands of people who get acne are especially sensitive to a hormone called testosterone. This causes the glands to pump out an excess of oil. At the same time, the dead skin cells lining the openings of the hair follicles are not shed properly and clog up the follicles. These two effects combine to cause a build up of oil within the hair follicles. The acne bacteria live on everyone’s skin, usually causing no problems, but in those who are prone to acne, the build up of oil creates an ideal environment in which these bacteria can multiply. This triggers a chemical reaction and the formation of red or pus-filled spots. Sometimes the blocked follicles do not become inflamed. The term ‘blackhead’ is used when the blockage can be seen as a dark plug at the skin surface. A bumpy and flesh coloured blocked follicle lying just under the skin is called a ‘whitehead’.
Your body makes more androgen hormones as teenagers, under stress, before menstruation, with dairy produce, medicines and contraceptives and, during and after pregnancy.
- Androgens increase sebaceous oil gland activity
- Skin cells block sebaceous oil ducts – blackheads and whiteheads
- Acne bacteria multiply behind block
- Bacteria cause inflamed spots
Is acne hereditary?
Acne can run in families, but this does not necessarily mean that if your parents had acne you will get it too.
Acne in young children
Recent studies have shown that puberty is beginning earlier and earlier in today’s children and preteen acne is on the rise in children ages 10-12, and sometimes in those even younger. It brings with it many changes and among them, is acne. The onset and duration of puberty depends on many things including gender, nutrition and ethnicity. Girls usually begin puberty between the ages of 10-14 and boys will begin between the ages of 12-16.
How is acne diagnosed?
Acne is easily recognised by the appearance of the spots and by their distribution on the face, neck, chest or back. However, there are several varieties of acne and your dermatologist will be able to tell you which type you have after examining your skin. The most common type is called ‘acne vulgaris ‘.
How acne develops
From Androgens;
- Teenage hormones
- Stress
- Diet
- Hormone contraceptives
- Pregnancy
- Post pregnancy
- Perimenopausal acne
Other;
- Comedogenic creams & cosmetics
- Acne causing Medicines
- Friction from clothes, sweat bands etc
- Hormone Replacement Therapy (HRT)
- Testosterone therapy
Ages of acne
Studies in the 1970’s showed the peak-incidence for acne was the late teens and the incidence reduced with age. Male patients were more frequently affected and had more severe forms of acne. Johnson MT, Roberts J Vital Health Stat USA 1978 Cunliffe W, Gould DJ Br Med J 1979 1,1109-1110
In the 21st century, acne has become more than a teenage problem.
- 25% of acne start in adults
- Over ⅓ of women in their 30’s have acne.
Research studies show that the adult onset of acne:
Occurs in 54% of women and 40% of men
Late onset can in women over 20 is increasing and more likely to persist.
Acne in adult women tends to differ from that seen in teenagers with more inflammatory papules and pustules and fewer comedomes, frequently on the lower face and jawline.
Diet is linked with acne
Recent research suggests that some people get acne worse after consuming certain foods e.g. foods high in sugars, high ‘glycemic foods’ e.g. sweets. Also some milk products.
The association between acne and dairy consumption has been subject to large studies.
A four month study demonstrated that individuals with acne consumed a diet of high GI index foods (white bread, potatoes, rice) and greater amounts of milk and dairy ice-cream compared with controls.
Male acne patients had lower lesion count on a low GI diet for 12 weeks.
Some populations have no acne
No acne was found in 1200 Kitavan islanders in Papua New Guinea, nor in the Aiche tribe in Paraguay. This is possibly due to no dairy, low GI, non western diets.
Can acne be cured?
Several types of treatment may improve or clear acne, but acne may go into remission (clearance) after treatment. The aims of treatment are to prevent new spots forming, to improve those already present and to prevent scarring.
How can acne be treated?
If you have acne, but have had no success with over the counter products, then it is probably time for you to visit your doctor. However it is unrealistic to expect overnight cures. In general, most treatments take two to four months to produce their maximum effect.
Acne treatments fall into the following categories:
- Topical treatments (those that are applied directly to the skin) both non prescription creams, gels, washes etc and prescription creams, gels, washes etc.
- Oral antibiotics (tablets taken by mouth).
- Oral hormone blocking tablets to reduce hormonal acne.
Isotretinoin capsules (RoAccutane) to improve and in 70% of patients leave them clear at the end of a course of treatment.

Acne in Adult Woman
Other treatments.
Topical treatments: These are applied directly to the skin and include a variety of active anti-acne ingredients such as salicylic acid, benzoyl peroxide, niacinamide, antibiotics, azelaic acid and retinoids. Topical treatments are usually the first choice for people with mild to moderate acne. They should be applied to the whole of the affected area and not just to the spots themselves. Some of these should be avoided during pregnancy.
Oral antibiotic treatment: Your doctor may recommend a course of antibiotic tablets, which will be taken in combination with suitable topical treatment. Oral antibiotics help the inflamed acne spots but have no effect on uninflamed ones such as blackheads. Blackheads are helped by gels and creams containing salicylic acid and retinoids. They are suitable for widespread acne because topical treatments may then be difficult to apply properly to all of the affected areas. Antibiotics need to be taken for at least three months and are usually continued until there is no further improvement. Most oral antibiotics should not be taken if you are pregnant or planning a pregnancy.
Oral hormone blocking tablets: Spironolactone is a medicine that can reduce the effects of your androgen hormones on the overactive oil glands that lead to acne. It is also used as a diuretic ‘water pill’ at higher doses. It may make your periods irregular. Spironolactone cannot be taken if you are pregnant or planning a pregnancy. Some oral contraceptive pills such as Yasmin also block the hormone effects on the oil glands. Risks need to be discussed with your doctor.
Isotretinoin (e.g. RoAccutane): This powerful treatment acts directly on the oil producing glands and can be prescribed only by a dermatologist. Isotretinoin can harm an unborn child. Pregnancy tests will therefore be performed before starting treatment and throughout treatment and must have been shown to be negative on two occasions four weeks apart before you can start the treatment. You must also use effective contraception whilst on the treatment and for five weeks afterwards. Recent concerns regarding depression and suicidal feelings may worry some patients. A careful, in-depth consultation will take place before a course of treatment starts. Dr Lowe routinely starts patients on low dose RoAccutane to reduce the side effects. The dose is then gradually increased. You cannot fall pregnant whilst taking this medication or for one month after stopping RoAccutane.

Severe acne treated with RoAccutane
Other treatments; Lights lasers and Peels: Our clinic offers other acne treatments which includes light and laser therapy, various chemical peels, Dermasweep and gentle microdermabrasion. Light and laser treatments for acne can be helpful to reduce inflamed acne.
However your acne affects you, it is important to take action and start on treatment to control it as soon as it appears. This helps to avoid permanent scarring and reduces embarrassment.
Expect to use your treatments for at least two months before you see steady improvement. Make sure you understand how to use them correctly so you get the maximum benefit.
Some topical treatments may dry or irritate the skin when you start using them. An oil free moisturiser should help, but you may also have to cut down the frequency with which you put the treatment on.
Wear oil-free, water-based make-up and choose products that are labelled as being ‘non-comedogenic’ (should not cause whiteheads or blackheads) or ‘non acnegenic’ (should not cause acne). Remove them at night with a gentle cleanser and water. Scrubbing too hard can irritate the skin and make your acne worse.
An acne treatment programme, for example our Cranley Clinic Acne Protocol with our medical aestheticians can help. This programme usually consists of; visible red light therapy, various peels, microdermabrasion, and acne surgery (steam and extraction). The programme will vary from patient to patient.

Remember that squeezing spots usually
aggravates them
Non-Prescription products include:
AcclenzTM Purify and Renew Foaming Cleanser
AcclenzTM Deep Down Cleansing Mask
AcclenzTM Advanced Action Spot Gel
AcclenzTM Oil Control Day Cream
AcclenzTM Deep Action Blemish Serum
Panoxyl Wash
Dermol 500 Lotion
Possible future acne treatments
- New oral antibiotics, Sarecycline
- New topical antibiotics, Minocycline
- Nitric oxide gels
- Sebum inhibitors
- Anti microbial peptides

